Chronic Fatigue Syndrome & Long COVID Understanding the Overlap
Chronic fatigue syndrome long covid – Chronic fatigue syndrome (CFS) and long COVID share a disturbing overlap in symptoms, impacting daily life in profound ways. This exploration delves into the defining characteristics, potential underlying mechanisms, and the substantial impact these conditions have on individuals’ well-being.
From defining the distinct and overlapping symptoms to examining the diagnostic challenges, this blog post thoroughly investigates chronic fatigue syndrome and long COVID, exploring the similarities and differences between these conditions. We’ll also touch upon the treatments, research, and future directions in the quest for better understanding and management.
Defining Chronic Fatigue Syndrome (CFS) and Long COVID
Chronic Fatigue Syndrome (CFS) and Long COVID are complex conditions that affect millions worldwide. Understanding their similarities and differences is crucial for accurate diagnosis and effective treatment. Both conditions are characterized by debilitating fatigue, but their underlying causes and symptom profiles can vary. This exploration will delve into the definitions, characteristics, diagnostic criteria, and clinical presentations of CFS and Long COVID, highlighting the overlapping features and distinctions between them.
Defining Chronic Fatigue Syndrome (CFS)
Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME), is a debilitating illness primarily characterized by persistent and overwhelming fatigue. This fatigue is often described as different from simple tiredness, and significantly interferes with daily activities and quality of life. The fatigue is often accompanied by a range of other symptoms, including muscle pain, cognitive difficulties (brain fog), sleep disturbances, and headaches.
Key Characteristics and Symptoms of CFS
The hallmark symptom of CFS is profound and persistent fatigue. This fatigue is not relieved by rest and can significantly impair a person’s ability to function. Other common symptoms include:
- Muscle pain (myalgia) and/or joint pain (arthralgia).
- Cognitive difficulties, such as problems with memory, concentration, and processing information (often referred to as “brain fog”).
- Sleep disturbances, including difficulty falling asleep, staying asleep, or experiencing restorative sleep.
- Headaches and other neurological symptoms.
- Sore throat, tender lymph nodes, and other flu-like symptoms.
Diagnostic Criteria for CFS, Chronic fatigue syndrome long covid
Diagnosis of CFS is challenging due to the lack of specific laboratory tests. The diagnostic criteria typically involve a combination of symptoms and exclusion of other conditions. The most commonly used criteria, the Fukuda criteria, require the presence of persistent fatigue for at least six months, accompanied by at least four of eight associated symptoms. Important distinctions exist when comparing CFS with other conditions, such as fibromyalgia and depression.
Overlapping symptoms can lead to diagnostic confusion, and accurate diagnosis often requires a careful and comprehensive evaluation by a healthcare professional.
Ugh, chronic fatigue syndrome and long COVID are seriously draining. It’s hard to even keep up with the daily grind, let alone the news. Hearing about the recent shooting on the D train in NYC, nyc shooting d train , really highlights how unpredictable life can be. It’s another layer of stress on top of everything else, which just makes managing these chronic illnesses even tougher.
I’m hoping for better days, and maybe some peace of mind soon.
Understanding Long COVID’s Clinical Presentation
Long COVID encompasses a wide range of symptoms experienced by individuals who have had a confirmed or suspected COVID-19 infection. These symptoms can manifest months after the initial infection and can vary greatly in severity and duration. A common theme is the persistent nature of the symptoms. Similar to CFS, long COVID often presents with fatigue as a primary complaint, but the symptoms can also include:
- Respiratory problems (e.g., shortness of breath, cough).
- Cardiovascular issues (e.g., palpitations, chest pain).
- Neurological problems (e.g., headaches, dizziness, brain fog).
- Gastrointestinal problems (e.g., diarrhea, abdominal pain).
Comparing Diagnostic Processes for CFS and Long COVID
The diagnostic processes for both CFS and Long COVID rely heavily on a comprehensive evaluation of symptoms, medical history, and exclusion of other potential causes. For CFS, the Fukuda criteria are commonly used, while no single, universally accepted diagnostic criteria exist for Long COVID. Current approaches emphasize symptom reporting, physical examinations, and exclusion of alternative diagnoses. A key difference lies in the recognition of a possible link to a previous COVID-19 infection in the case of Long COVID, whereas in CFS, the cause remains largely unknown.
Summary Table
| Feature | Chronic Fatigue Syndrome | Long COVID | Overlap |
|---|---|---|---|
| Symptoms | Persistent fatigue, muscle pain, cognitive difficulties, sleep disturbances, headaches, flu-like symptoms | Persistent fatigue, respiratory problems, cardiovascular issues, neurological problems, gastrointestinal problems | Fatigue, cognitive difficulties, headaches, and other systemic symptoms |
| Diagnostic Criteria | Fukuda criteria, symptom duration, exclusion of other conditions | Symptom reporting, medical history, exclusion of alternative diagnoses, potential link to COVID-19 infection | Emphasis on symptom duration and exclusion of other conditions |
Underlying Mechanisms: Chronic Fatigue Syndrome Long Covid
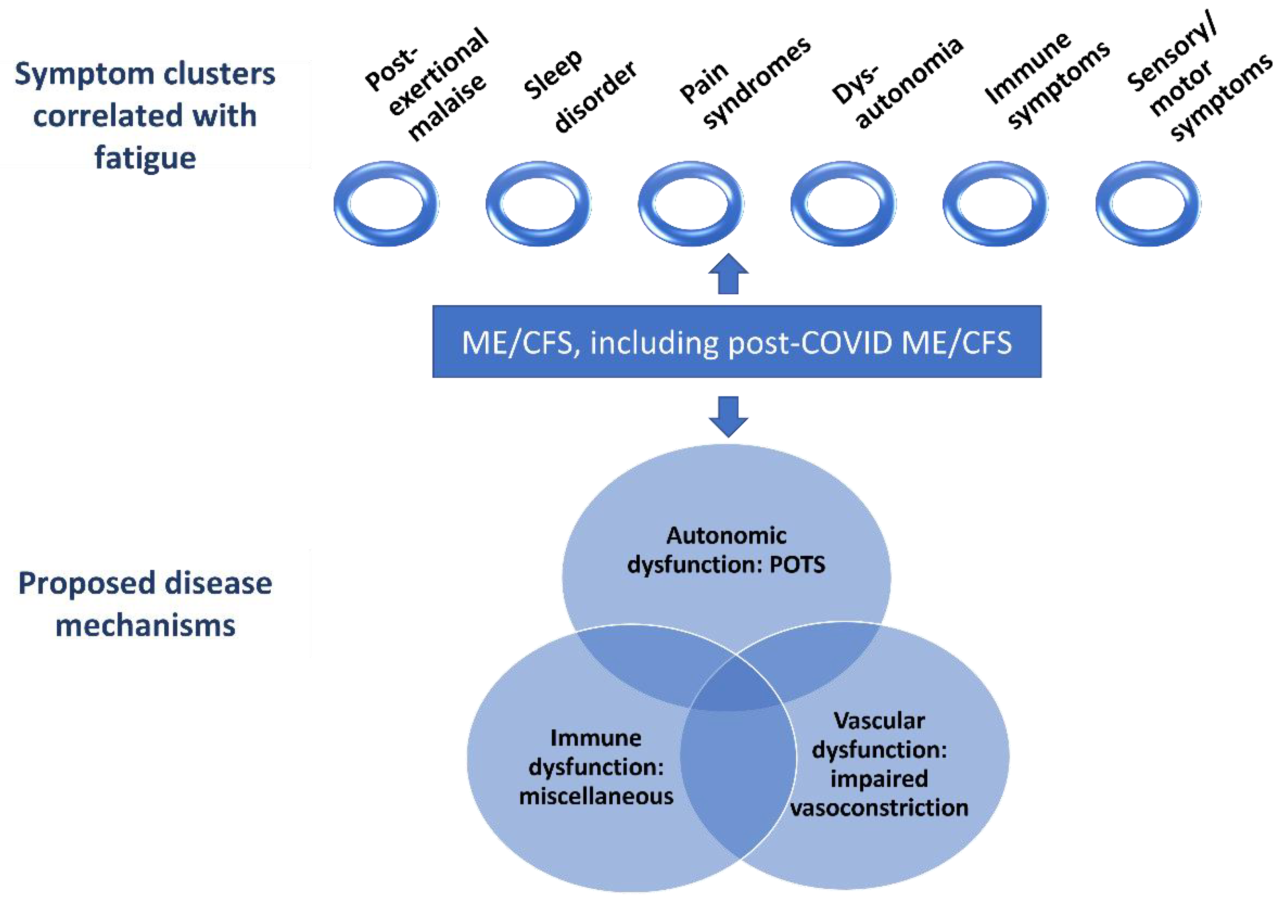
Chronic Fatigue Syndrome (CFS) and Long COVID, while distinct conditions, share overlapping biological pathways. Understanding these mechanisms is crucial for developing effective treatments and improving the lives of those affected. Both conditions are characterized by debilitating fatigue, but the underlying causes remain complex and not fully understood. Research continues to unravel the potential pathways involved, leading to a clearer picture of the intricate interplay of factors that contribute to these conditions.The proposed biological mechanisms behind CFS are diverse and not definitively established.
However, several key areas of investigation include inflammation, immune dysregulation, and potential neurological involvement. Similarly, the mechanisms linking viral infections, particularly SARS-CoV-2, to Long COVID are also under intense scrutiny. Research highlights a range of potential factors, including the persistent immune response to the virus, direct tissue damage, and the complex interplay between the immune system and the nervous system.
Inflammation
Inflammation plays a significant role in both CFS and Long COVID. Chronic low-grade inflammation, characterized by elevated levels of inflammatory markers, is observed in individuals with both conditions. This persistent inflammatory response can contribute to tissue damage, fatigue, and other symptoms. The exact triggers and mechanisms driving this inflammation are not fully understood.
Immune Dysregulation
Immune dysregulation is another crucial aspect of both conditions. In CFS, immune cells may exhibit abnormal activation and function, leading to an overactive or underactive immune response. This dysregulation can result in an inappropriate inflammatory response and contribute to the development of symptoms. In Long COVID, a persistent immune response to the SARS-CoV-2 virus may trigger immune dysfunction, including autoimmunity, where the immune system attacks the body’s own tissues.
Oxidative Stress
Oxidative stress, an imbalance between reactive oxygen species (ROS) and antioxidant defenses, is implicated in both CFS and Long COVID. This imbalance can lead to cellular damage and contribute to various symptoms. Increased ROS levels may exacerbate inflammation and immune dysregulation, further contributing to the development of chronic symptoms.
Neurological Involvement
Neurological involvement is a significant consideration in both conditions. Symptoms such as brain fog, cognitive dysfunction, and sleep disturbances are common in CFS and Long COVID. Research suggests that inflammation and immune dysregulation may directly impact the nervous system, leading to structural or functional changes. These changes may contribute to the cognitive and neurological symptoms experienced by individuals with both conditions.
Overlap in Underlying Mechanisms
The overlap in potential underlying mechanisms between CFS and Long COVID is substantial. Both conditions often involve chronic inflammation, immune dysregulation, and oxidative stress. While the specific mechanisms and their relative importance may vary, the shared pathways highlight the potential for common treatment strategies and further research into shared biological pathways. For instance, treatments targeting inflammation and immune function may prove beneficial in both conditions.
Chronic fatigue syndrome and Long COVID can be incredibly isolating, leaving sufferers feeling like they’re adrift in a sea of exhaustion. The recent news of the couple missing from their boat in Grenada, highlights the profound impact that unexpected circumstances can have on individuals and families. Navigating these challenging health conditions requires immense resilience, just like the search for the missing couple in the Caribbean, which underscores the need for ongoing support and research into these conditions like chronic fatigue syndrome and long COVID.
couple missing boat grenada It’s a sobering reminder of the unpredictable nature of life, and the ongoing need for compassion and understanding in our communities.
Comparison of Mechanisms
| Mechanism | Chronic Fatigue Syndrome | Long COVID |
|---|---|---|
| Inflammation | Chronic low-grade inflammation, elevated inflammatory markers, potential involvement of various cytokines. | Persistent inflammatory response to SARS-CoV-2, potential involvement of specific viral components, potential immune-mediated inflammation. |
| Immune Dysregulation | Abnormal activation and function of immune cells, potential autoimmunity, inappropriate immune response. | Persistent immune response to SARS-CoV-2, potential immune cell dysfunction, potential autoimmunity directed at host cells. |
Impact on Daily Life
Living with chronic fatigue syndrome (CFS) or Long COVID significantly alters daily life, impacting everything from work and social interactions to personal relationships and overall well-being. The unpredictable nature of these conditions often leads to significant functional limitations, making even simple tasks feel overwhelming. This chapter explores the profound effects on daily activities and quality of life, highlighting the common challenges faced by individuals living with these conditions.The daily lives of individuals with CFS and Long COVID are frequently characterized by a fluctuating energy level, cognitive impairments, and physical limitations.
These factors make it difficult to maintain consistent routines, participate in social activities, and engage in work or other responsibilities. Understanding these impacts is crucial for developing effective support strategies and interventions.
Impact on Work
The fluctuating nature of symptoms in both CFS and Long COVID makes consistent employment challenging. Many individuals experience significant limitations in their ability to focus, concentrate, and maintain sustained effort, impacting productivity and job performance. Employers may not always understand the invisible nature of these conditions, leading to misunderstandings or even job loss. Furthermore, the unpredictable nature of symptoms can lead to missed workdays, impacting income and career progression.
Chronic fatigue syndrome and Long COVID are serious conditions that often leave sufferers struggling with debilitating symptoms. The recent Disney World allergy death lawsuit highlights the potential dangers of inadequate allergy management in public spaces, raising important questions about safety protocols. Understanding the factors contributing to such tragedies, like the ones seen in disney world allergy death lawsuit , is crucial for developing better preventative measures for those with chronic health conditions like chronic fatigue syndrome and Long COVID.
These conditions often require careful management and proactive support to prevent similar outcomes.
- Reduced productivity and efficiency: Individuals may struggle to complete tasks, meet deadlines, or maintain consistent output. This can stem from cognitive fog, fatigue, and physical limitations.
- Missed workdays and absenteeism: The unpredictability of symptoms often leads to missed workdays, impacting income and potentially jeopardizing employment.
- Difficulty maintaining a consistent work schedule: The fluctuating energy levels associated with CFS and Long COVID can make it challenging to maintain a regular work schedule, leading to increased stress and difficulty in meeting work demands.
- Job loss or career limitations: Due to persistent symptoms and difficulty performing job duties, some individuals may experience job loss or be forced to change careers or accept less demanding roles.
Impact on Social Life
Social activities, often a crucial aspect of well-being, can become significantly affected for those with CFS and Long COVID. The energy expenditure and cognitive challenges associated with these conditions can make it difficult to participate in social events, maintain friendships, or engage in recreational activities.
Chronic fatigue syndrome, often overlapping with long COVID, can leave sufferers feeling utterly drained. The recent tragic events surrounding the armorer Alec Baldwin’s Rust shooting incident, armorer alec baldwin rust shooting , serve as a stark reminder of how even seemingly unrelated tragedies can impact our collective well-being, and highlight the need for increased support for those suffering from these debilitating conditions.
- Reduced social participation: Fatigue, pain, and cognitive difficulties can make attending social gatherings, maintaining friendships, or pursuing hobbies a significant challenge.
- Isolation and loneliness: The need to limit social interactions due to symptom fluctuations can lead to feelings of isolation and loneliness.
- Difficulty maintaining relationships: The fluctuating nature of the conditions can impact communication and understanding within personal relationships, leading to strain or conflict.
- Strain on social support networks: The ongoing demands of the conditions can strain social support networks, leading to feelings of burden or resentment.
Impact on Relationships
Personal relationships can also be significantly affected by CFS and Long COVID. The unpredictable nature of symptoms, the need for rest and recovery, and the strain on energy levels can lead to challenges in communication, intimacy, and overall connection.
- Communication difficulties: The cognitive fog and fatigue associated with these conditions can make communication challenging, leading to misunderstandings or conflict.
- Strained intimacy: The physical and emotional toll of these conditions can impact intimacy and closeness in personal relationships.
- Impact on family dynamics: The need for accommodations and support can impact family dynamics, requiring adjustments to daily routines and responsibilities.
- Increased burden on caregivers: Caregivers may experience increased stress and burden in supporting individuals with these conditions.
Comparison Table
| Life Aspect | CFS Impact | Long COVID Impact |
|---|---|---|
| Work | Reduced productivity, missed workdays, difficulty maintaining consistent schedules, potential job loss or career limitations. | Reduced productivity, difficulty concentrating, missed workdays, potential job loss or career limitations, and often exacerbated by cognitive dysfunction. |
| Social Life | Reduced participation in social activities, potential isolation and loneliness, strained relationships. | Reduced participation in social activities, potential isolation and loneliness, difficulty maintaining friendships and relationships, and often exacerbated by post-viral fatigue. |
| Relationships | Communication difficulties, strained intimacy, impact on family dynamics, increased burden on caregivers. | Communication difficulties, strained intimacy, impact on family dynamics, increased burden on caregivers, and often exacerbated by emotional and mental health challenges. |
Treatment and Management Strategies

Navigating chronic fatigue syndrome (CFS) and Long COVID often feels like an uphill battle. While there’s no cure for either condition, effective management strategies can significantly improve quality of life. Understanding the available treatments and their potential impact is crucial for developing a personalized approach.Treatment options for CFS and Long COVID vary widely, reflecting the complex nature of these conditions.
Success often hinges on a holistic approach that combines various therapies tailored to individual needs.
Current Treatment Options for CFS
Currently, there’s no single, universally effective treatment for CFS. Management focuses on alleviating symptoms and improving overall well-being. A variety of pharmacological interventions and lifestyle modifications are employed.Pharmacological interventions may include medications to manage pain, sleep disturbances, or other associated symptoms. However, their effectiveness can vary greatly depending on the individual. Some research suggests that certain antidepressants and anti-inflammatory medications may help reduce fatigue in some individuals.
Available Management Strategies for Long COVID
Long COVID presents a unique set of challenges in terms of treatment. Management often involves a multifaceted approach tailored to the specific symptoms and their impact on daily life.Many patients find relief through lifestyle modifications, including regular exercise (with careful consideration for individual tolerances), healthy eating, and adequate sleep. Furthermore, cognitive behavioral therapy (CBT) and other psychological interventions can help manage anxiety, depression, and the emotional toll of the condition.
Early intervention and support are vital.
Commonalities and Differences in Treatment Approaches
Both CFS and Long COVID share a common thread of symptom management, emphasizing the importance of personalized care. However, differences arise from the diverse range of symptoms experienced by individuals. While some pharmacological interventions might show promise in both, the specific medications and their effectiveness may vary considerably.Long COVID often involves a broader range of symptoms, including neurological issues and cardiovascular problems.
These specific needs require a more comprehensive and tailored approach to management. CFS, on the other hand, primarily focuses on alleviating fatigue and other chronic symptoms.
Importance of Multidisciplinary Care
Given the complexity of these conditions, a multidisciplinary approach is paramount. A team of healthcare professionals, including physicians, therapists, and specialists in related fields, can offer a more comprehensive and effective strategy.This approach allows for a holistic assessment of the patient’s needs, considering physical, psychological, and social factors. Communication and collaboration between specialists are crucial for developing a personalized treatment plan.
Chronic fatigue syndrome and long COVID can really take a toll, impacting everything from daily life to financial stability. Suddenly, navigating the rising costs of living, like those associated with finding an affordable home, becomes incredibly challenging, especially in places like California where 800000 dollar homes california are becoming increasingly common. This makes managing the ongoing health impacts of these conditions even more difficult.
It’s a complex issue, and there’s still a lot we don’t understand.
Key Strategies for Managing Both Conditions
A structured approach is vital for managing both CFS and Long COVID. These conditions often require long-term management, and a patient-centered approach is critical.
- Regular monitoring of symptoms: Tracking symptoms, including fatigue levels, pain, and other physical or mental health changes, provides valuable data for adjusting treatment plans. This can help in understanding how various factors affect symptoms and can aid in communicating effectively with healthcare professionals.
- Gradual lifestyle adjustments: Introducing changes in diet, exercise, and sleep patterns gradually, rather than abruptly, can help minimize potential adverse reactions and ensure sustainable improvements. Gradual adjustments are more likely to be successful and less disruptive.
- Seeking support from a multidisciplinary team: Engaging a team of specialists, including physicians, therapists, and specialists in related fields, ensures comprehensive care and a coordinated approach.
Summary of Available Treatments
| Treatment Approach | Chronic Fatigue Syndrome | Long COVID |
|---|---|---|
| Pharmacological Interventions | Antidepressants, anti-inflammatory medications (effectiveness varies widely), medications for pain and sleep disturbances. | Medications for specific symptoms (e.g., pain relievers, blood thinners for some cases), and some antiviral medications for early intervention (effectiveness is still being investigated). |
| Lifestyle Modifications | Gradual exercise, dietary adjustments, sleep hygiene, stress management techniques. | Gradual exercise, dietary adjustments, sleep hygiene, stress management techniques, and managing cognitive dysfunction. |
Research and Future Directions
Unraveling the mysteries of chronic fatigue syndrome (CFS) and Long COVID requires sustained and focused research. Current efforts are exploring potential underlying mechanisms, diagnostic criteria, and effective treatments. The complexity of these conditions necessitates collaboration among researchers, clinicians, and patients to accelerate progress. The future of research in this area hinges on innovative approaches and a commitment to understanding these debilitating illnesses.
Ongoing Research into CFS
Current research into CFS is multifaceted, encompassing various avenues of investigation. Studies are examining the potential role of inflammation, immune dysregulation, and mitochondrial dysfunction in the development and progression of CFS. Researchers are also exploring the genetic predisposition to CFS and identifying potential biomarkers for diagnosis and prognosis. These investigations aim to move beyond symptom-based diagnoses towards a more mechanistic understanding of the condition.
Current Research Efforts Focusing on Long COVID
Long COVID research is intensely focused on identifying the diverse range of lingering symptoms and their potential causes. Studies are analyzing the impact of the virus on various organ systems, looking at how the immune response might contribute to persistent symptoms. Researchers are also working to establish robust diagnostic criteria for Long COVID, moving away from relying solely on symptom lists.
Potential Areas for Future Research
Future research into CFS and Long COVID should concentrate on developing targeted therapies based on the underlying mechanisms identified in current studies. This could involve exploring new drug treatments or repurposing existing medications to address specific aspects of the illness. Developing standardized diagnostic tools that are more accurate and reliable than existing methods is crucial. This would aid in early identification and appropriate management of these conditions.
Another important avenue for research is the exploration of environmental factors that might influence the development or severity of CFS and Long COVID.
Areas Where Research Efforts Need to Focus
A significant area needing increased focus is the development of robust and standardized outcome measures for evaluating treatment efficacy. Currently, the assessment of treatment responses is often inconsistent, hindering the ability to objectively compare different interventions. Furthermore, there is a need for more longitudinal studies to track the long-term course of CFS and Long COVID, which can provide valuable insight into disease progression and the impact on quality of life.
Importance of Research Collaboration
Collaboration between researchers from different disciplines, including immunologists, virologists, neurologists, and psychiatrists, is paramount. Sharing data, expertise, and resources is essential to accelerate progress. Moreover, patient involvement in research is crucial. Collecting patient experiences and perspectives can provide invaluable insights into the lived realities of these conditions and help tailor research priorities to better meet patient needs.
Patient advocacy groups play a vital role in facilitating this collaboration.
Future Research Directions for CFS and Long COVID
- Developing and validating new diagnostic tools based on objective biological markers.
- Identifying and characterizing specific immune dysfunctions that contribute to the development and persistence of symptoms.
- Investigating the role of gut microbiome in CFS and Long COVID, exploring potential therapeutic interventions targeting the gut microbiome.
- Exploring the role of environmental factors, such as exposure to toxins or infections, in triggering or exacerbating CFS and Long COVID.
- Developing targeted therapies to address specific underlying mechanisms of the conditions, moving beyond symptom-based treatments.
- Establishing standardized outcome measures for evaluating treatment effectiveness.
- Conducting longitudinal studies to track long-term outcomes and monitor the impact on quality of life.
- Improving access to high-quality, comprehensive care for patients.
- Promoting research collaboration among scientists, clinicians, and patients to foster a more holistic approach to understanding and managing these conditions.
Final Summary
In conclusion, chronic fatigue syndrome and long COVID, while distinct conditions, share significant overlap in symptoms, underlying mechanisms, and impact on daily life. Further research, collaborative efforts, and improved diagnostic tools are crucial for better understanding and ultimately, more effective treatment and management strategies for both conditions. The journey toward better outcomes necessitates a multidisciplinary approach.
FAQ Overview
What are some common symptoms that overlap between CFS and Long COVID?
Fatigue, muscle pain, cognitive difficulties, sleep disturbances, and headaches are some of the overlapping symptoms frequently reported by individuals experiencing either CFS or Long COVID.
How do the diagnostic criteria differ between CFS and Long COVID?
While both conditions require a detailed medical evaluation, the diagnostic criteria for CFS are more focused on symptom duration and exclusion of other conditions, whereas Long COVID’s diagnosis is often linked to a recent SARS-CoV-2 infection.
Are there any promising new treatments being researched for CFS and Long COVID?
Research is ongoing into various treatment approaches, including pharmacological interventions, lifestyle modifications, and therapies targeting inflammation and immune dysregulation. These are still in early stages of development.
What role does the immune system play in both CFS and Long COVID?
Both conditions exhibit signs of immune dysregulation, where the immune system may be overactive or underactive, leading to inflammation and various downstream symptoms.

